What is Osteoporosis
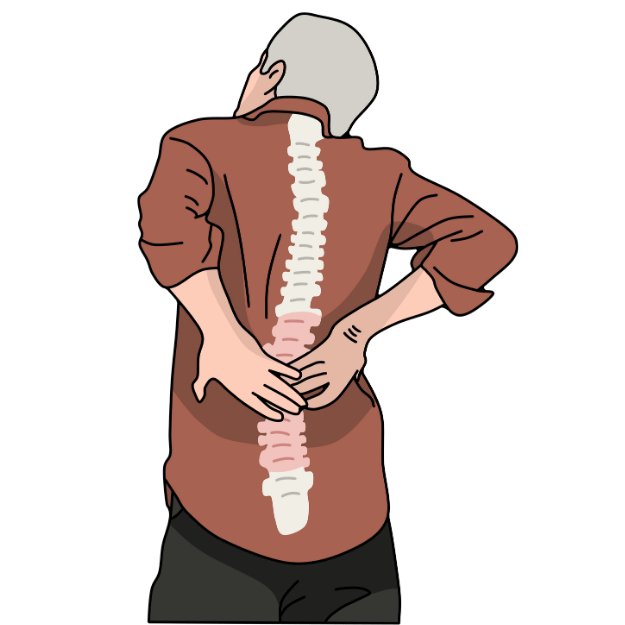
Osteoporosis is a progressive bone disease characterised by reduced bone density and bone deterioration that makes the bones fragile and more susceptible to fractures. Osteoporosis translates to “porous bone” and occurs when bone creation cannot keep up with bone loss. It is a silent disease, as it typically has no symptoms until a fracture occurs.
Osteoporosis impacts over 900,000 Australians. One in three women and one in five men experience an osteoporotic fracture - caused by weak bones - during their lifetime. Diagnosis typically occurs after menopause for women and after age 70 for men. However, the foundation for bone health is built throughout life, and preventive strategies are critical for all adults.
The condition primarily affects the spine, hips and wrists. Fractures in these areas can cause significant reductions in mobility and quality of life. Hip fractures are particularly concerning - 20% of people die within the first year following a hip fracture, and many more have significant mobility and independence loss. Prevention and early detection can help slow bone loss and significantly reduce the risk of fractures.